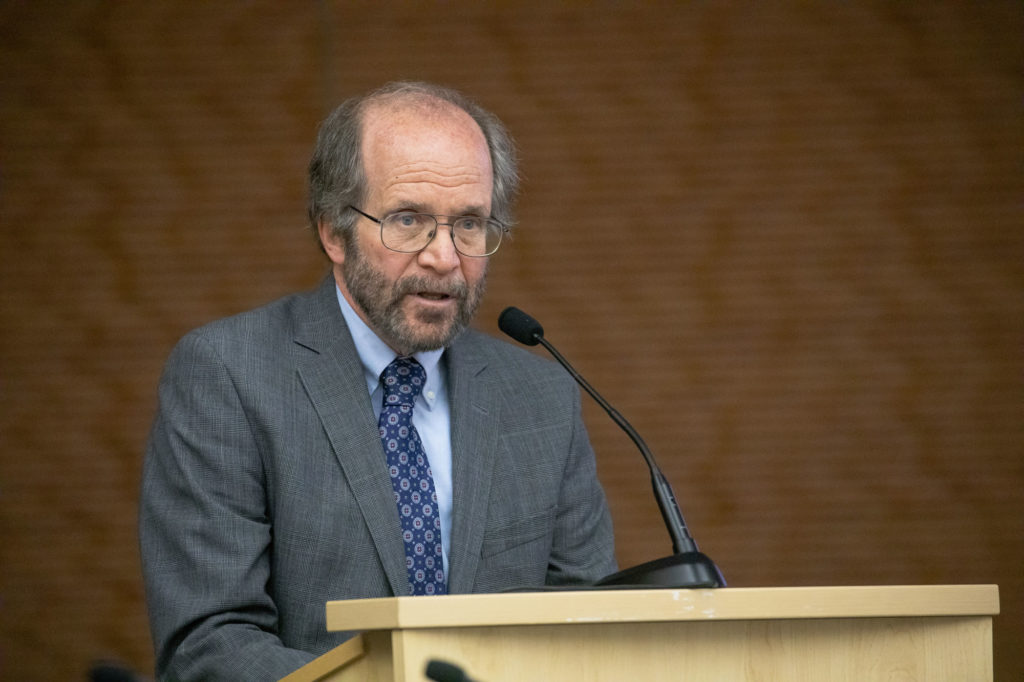
Photos by Craig Wild/UW-Madison
Dr. Robert Golden, dean of the University of Wisconsin School of Medicine and Public Health, said the state needs to get in a better position when it comes to COVID-19 so it can handle the challenges that will come this fall, including the onset of flu season.
“We’re at a critical point now,” Golden told Wisconsin Health News Tuesday. “Things are not heading in the right direction and we’ve got to reverse course so that we enter into the challenges of fall and beyond with the right kind of momentum.”
Golden also said the University of Wisconsin-Madison’s plan for bringing undergraduates back this fall is “very thoughtful,” but that local and state governments have “to step up” with enforceable public health measures.
“If we don’t have all the public health measures in place, we are basically doing the equivalent of speeding down the highway without a seatbelt on,” he said. “Lives are at stake.”
Edited excerpts are below.
WHN: What is your assessment of the current situation?
RG: We are heading in the wrong direction. Now there is good news and bad news. The good news is that our state did a wonderful job early in the pandemic, relative to the rest of our nation…we really emphasized the simple, but effective public health measures – social distancing, wearing masks, shutting things down – so that we could put out the raging fire. We did a really good job in the beginning.
But I think through a various number of reasons, including the state Supreme Court decision about the limits of the governor’s authority, we are now in a backslide. I don’t think we are, to put it in perspective, in the kind of horrible, terrible shape that hotspots like Arizona and Florida are in. But we’re moving in the wrong direction, so that’s a great concern. We are not about to go over the cliff. But we’re slowly moving toward the cliff and that slow movement is beginning to gain speed rather than turning in the other direction.
So I think we’re at a really critical point. We have a little bit of time before some additional challenges come up, with things ranging from some more big traditional holidays of people gathering like Labor Day, with the anticipated return of college students throughout the state, throughout the region and the challenges with that, with the ever-present potential to begin to have supply chain problems, as our country, I hope, begins to aggressively ramp up testing so that it’s where it should have been all along. That might produce supply chain challenges for our own testing capacity within Wisconsin.
I would say the next four to six weeks are really, really important. We have to do everything we can to put the brakes on and head in the right direction.
WHN: Municipalities are enacting mask ordinances. Do you think that’s enough?
RG: No one measure is going to be effective. A combination of measures will also not be totally effective. But I can’t think of any rational reason, considering the life and death stakes that we’re playing with, that we shouldn’t do all the easy things. By easy things, I mean things that are not dependent on the whim of the virus or the challenges of a huge program to develop and deploy effective vaccines. So masks, socially distancing, adequate, effective contact tracing, adequate access to testing with turnaround times that are meaningful, meaning like a day or two rather than five to six days, which is the case in other parts of the country. All of that we should be doing right now.
We did very well in the beginning by having these unenforced mandates. And I think it’s because I think the people of Wisconsin are good, intelligent people who want to do what’s right for them, their families and their communities. But after a while, even good, well-intended people get exhausted and begin to stray in their voluntary compliance with things…I think that we now have to do all of the things in our toolkit that we have available and to do it in a way where there is a reasonable bit of oversight and enforcement so that blatant endangerment of the community is simply not allowed.
WHN: Last month, you laid out potential obstacles for vaccine development at a Wisconsin Manufacturers and Commerce webinar. What do you think of the development of a vaccine? Do you think it’ll be available in the timeframes that national officials have pointed to?
RG:
This field is changing on a daily basis. When I spoke earlier at the WMC, I was concerned that at that point, it seemed like pretty much the sole focus, or at least almost the sole focus, was on antibody protection, which is understandable. But there is another important component of immune responses and that’s the T cell response. And I was concerned because we were seeing individuals, who had recovered from clearly diagnosed COVID, and a short period out, they didn’t have any antibodies. That could mean really bad news, that people are almost, in a short period of time, susceptible to reinfection. Or it could be that people recovered primarily because of actions of other components of the immune system. So I was hoping that going forward, we would find a vaccine that would have a promising impact on both antibodies and also on T cells. And the news from (Monday) from England, suggests that there’s at least one vaccine that in a very preliminary way is suggesting it has an impact on those two Yin-Yang components of an effective immune response. So that is really good news. I’m really happy about that.
Not to be a pessimist, but rather to be a realist, we have a long way to go to cross the finish line with that and the other vaccines in development. Any one of them could suddenly go away as a viable potential if we discover, for example, a rare but significant, serious side effect or, in a larger scale, lack of effectiveness or that the virus, once exposed, has mutated forms that work around it, which is what we see very frequently with influenza, for example. Those concerns are just concerns to evaluate. I am very much more optimistic seeing the huge international effort to really go after this vaccine in a way that we haven’t seen in other perpetual viral illnesses. We still don’t have a vaccine for HIV, for example, and for other really deadly but rare diseases, whether it’s ebola or dengue. We still don’t have a vaccine. But I don’t think we had the incredible, international Blitzkrieg to develop a vaccine that we’re seeing now.
So I am increasingly optimistic that we will be moving into trials, perhaps as early as later in the fall and that we’ll find something that can be really ramped up for massive production and then dissemination. I really hope that we have the will as a nation to make sure that everybody gets the vaccine, that we put in the resources and the public education and maybe a public health imperative that people should get the vaccine. We can’t afford to have conspiracy theorists or the lack of financial resources or the lack of a well-trained, public health workforce stand in the way once we have this hoped-for magic bullet. We’ve got to make sure we can fire it. Otherwise all the sacrifice and all the hard work will be for vain.
WHN: What’s UW’s approach to a personalized medicine for COVID-19?
RB: There are many ways in which we are involved in that. So for example, we are looking at populations, including native populations and other populations that have health disparities that are once again getting disproportionately hammered by this particular epidemic as they have with other epidemics in the past. So we’re trying to learn more about it, not sort of at the typical personalized level of a given person, but at a somewhat broader, personalized approach to that particular population.
We are also studying the variations in the mutated strains that we can identify to see how they correlate with outcomes and to see if we can make any predictions about outcomes and effective preventions based on the personalized approach, looking at the infecting agent as opposed to looking at the individual. That’s some of the ways in which we’re doing it.
We are also, though, doing a lot of really exciting straight-up clinical trials with the treatments and gathering some additional biological information along the way so that we can retrospectively make it more personalized. I’m excited about our participation with one of these antibody cocktails. The one that we are particularly working with looks at neutralizing monoclonal antibodies, getting the ones that basic science suggests would be very helpful at blocking the spike protein and the viral interaction with human cells. So we’re involved in both preliminary phase one, two and three trials. We’re also doing a phase three randomized double blind trial as prophylactics for people who are at really high risk of exposure. So we’re excited about it.
We’re also looking at an existing drug, ruxolitinib, that is being repurposed to see if it can treat that horrible inflammatory cytokine storm. The first study, which we’re doing in partnership with others – this is a treatment that’s being developed by one of the big pharma companies – is to see if it works. But at the same time, we are gathering the information that retrospectively we can see in a personalized way, if it works better for some types of individuals versus other individuals.
WHN: What are the plans for medical school in the fall?
RG: Our situation with medical students is different than with undergraduates in most ways, not all ways. We never shut down our medical student education program. We really couldn’t without endangering the pipeline of physicians for our state and without disrupting the training of the individuals who were already here. And the same thing is true of the Medical College of Wisconsin and pretty much 90-plus percent of the medical schools in the country.
What we did do was immediately pull everybody away from the clinical training sites and switch overnight to online, virtual education. And that’s been going on without interruption from the very early start. We could do that for a while, but you can’t do that forever. You can’t even do that for too long because physicians have to get trained in medical school on actually examining, seeing and treating patients. The reasons why we pulled them initially were primarily in the early stages when we really didn’t know much about the epidemic to protect the safety and health of our students. But there was another reason. It was because we knew to have a measure of safety, they would have to have (personal protective equipment). And there wasn’t even enough for our doctors and nurses on the front lines. To further challenge the supply chain by bringing in the medical students just didn’t seem to make good public health sense…
Now they’re back at clinical training sites getting the intense clinical training with the extra precautions that are necessary, including making sure that they are screened every day when they show up to work at University Hospital or at other sites when we do our training and all of the other measures. So we think we are in OK shape for now. That’s assuming we don’t have a flare up again of supply chain challenges for PPE. But I think, for now, we’re pretty well stocked. It’s assuming that the epidemic doesn’t become horribly worse. If that happens, we’ll just have to figure out how to address that. Guiding all of this is the safety of our patients, the safety of our trainees and the faculty and the nurses.
This article first appeared in the Wisconsin Health News daily email newsletter. Sign up for your free trial here.