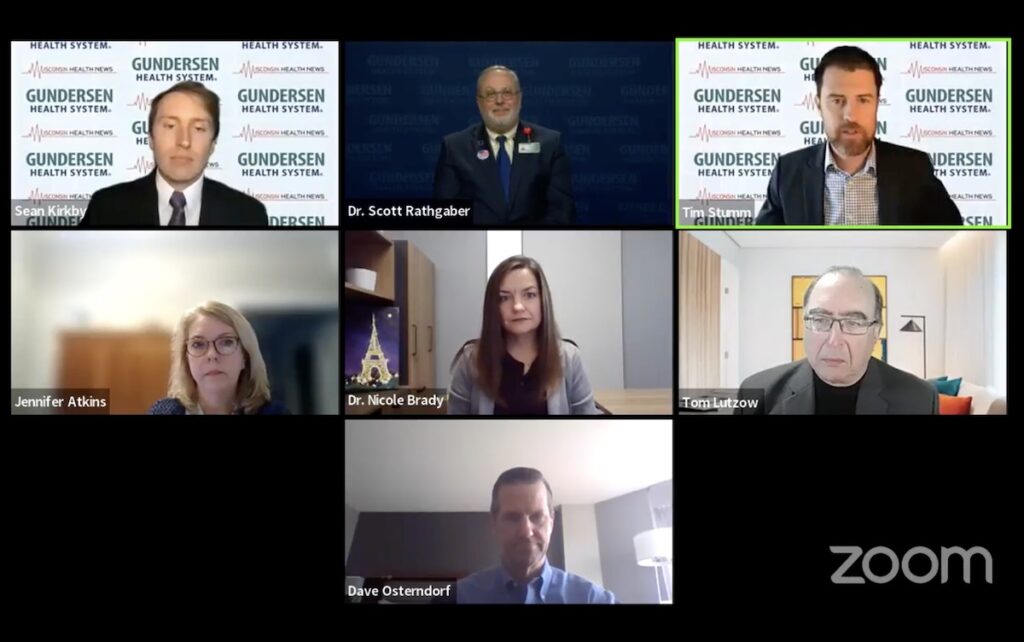
Trust among providers and payers is a key factor in the success of value-based contracts, panelists said Tuesday during a Wisconsin Health News virtual event.
“To get to that trust is part of the challenge,” said Tom Lutzow, a principal with Health Management Associates. “But, I think everyone wants to get there.”
Jennifer Atkins, senior vice president of managed care strategy for Advocate Aurora Health, said a lack of transparency is blocking some progress.
“Are things done in a black box behind the scenes? Or, are we able to see the attribution?” she said. “Are we able to see the quality performance, so that we can share that with our aligned and employed physicians so we can really drive what we all want to accomplish?”
Dr. Nicole Brady, chief medical officer for UnitedHealthcare’s employer and individual business in Wisconsin and Michigan, agreed that data-sharing is important.
“But a lot of this data contains either proprietary information or personal health information,” she said. “There are strict regulations on what you can or how you can share it, which can really be a burden when you’re trying to navigate these relationships.”
Data has been underutilized in healthcare, and that’s in part because different factions want to use it differently, according to Dave Ostendorf, Centivo’s chief actuary.
Often, if a group doesn’t like an outcome, they will blame the data, Ostendorf said. Meanwhile, he said employers are frustrated they don’t have more access to data.
“If value-based programs are going to work, everybody has to be moving in the same direction,” he said. “(It) needs to be on a collaborative basis and all parties need to understand what really is the deal and how it’s being measured.”