
CMS signs off on Medicaid work requirements
The Centers for Medicare and Medicaid Services signed off Wednesday on the state’s plans to require some childless adults on BadgerCare to work, making Wisconsin the fourth state to have current approval for Medicaid work requirements.
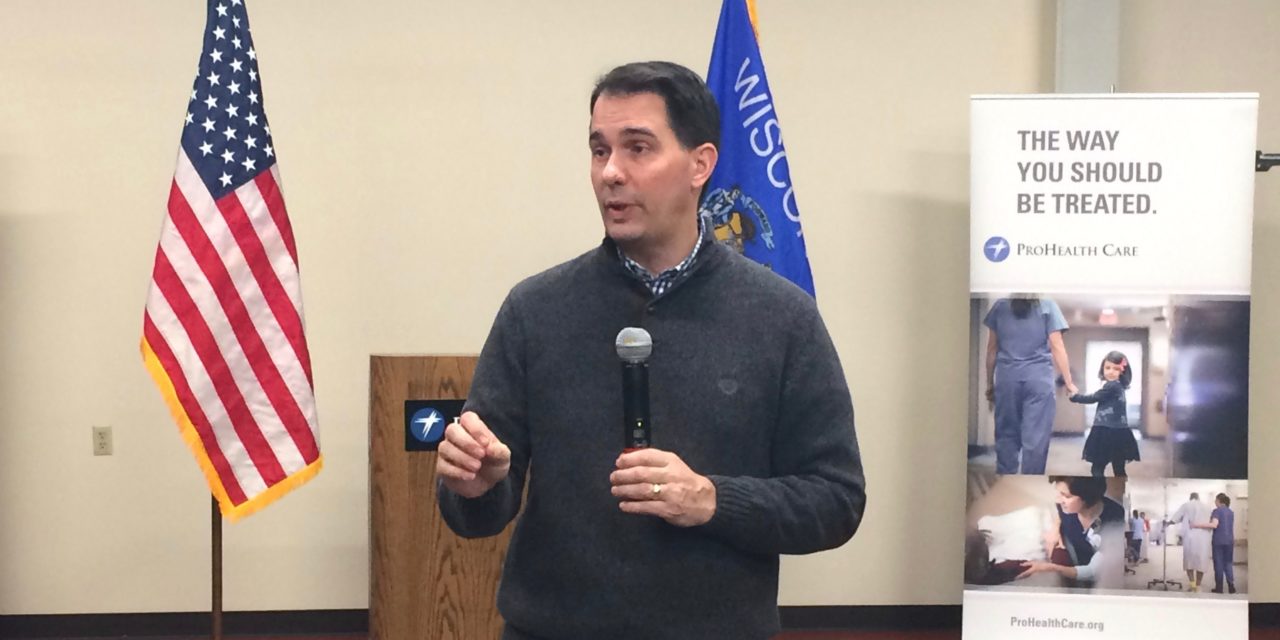
“With more people working in Wisconsin than ever before, we can’t afford to have anyone on the sidelines: we need everyone in the game,” Gov. Scott Walker said in a statement. “We want to remove barriers to work and make it easier to get a job, while making sure public assistance is available for those who truly need it.”
CMS approved Wisconsin’s current waiver, which was set to expire at the end of the year and allows the state to offer BadgerCare Plus to childless adults up to 100 percent of the federal poverty line.
It also signed off on a waiver amendment that would limit eligibility to four years for childless adults between the ages of 19 and 49 that do not meet work or community engagement requirements.
Under the waiver, adults in the program have to work, participate in worker training programs or be involved in “other community engagement” for at least 80 hours a month.
Once a member is out of compliance with that requirement for 48 months, they would lose eligibility for six months. They can re-apply for benefits after that, and the 48-month limit would reset.
The amendment also allows the program to charge childless adults making between 50 and 100 percent of the federal poverty level monthly premiums of $8. It also allows the program to charge an $8 copayment for using the emergency room in a non-emergency situation.
Members can reduce their premiums by making “healthy lifestyle choices,” like wearing a seatbelt, not smoking or maintaining a healthy weight, according to a statement.
Not included in the approved waiver are the state’s original plans to drug test beneficiaries. Instead, the waiver requires childless adults to complete a health and wellness questionnaire.
“Responses to questions on the (health risk assessment) will result in a referral for treatment, as applicable, but not impact an applicant’s Medicaid eligibility,” the waiver noted.
The amendment also provides full coverage for residential treatment of a substance use disorder.
The changes, except for the coverage of substance use disorder treatment, don’t affect the elderly, blind and disabled population or caretakers, children and pregnant women in the program.
The waiver also discontinues premiums for parents and caretakers who qualify for transitional medical assistance.
It’ll take at least a year to implement the policy changes, according to a statement. DHS is planning to work with members and stakeholders to get feedback to implement the plan.
“I support and share Gov. Walker’s commitment to helping adults on Medicaid achieve independence and self-sufficiency through community engagement,” CMS Administrator Seema Verma said in a statement. “I expect these reforms may serve as a model for states looking to tackle the drivers of poor health and improve outcomes for individuals.”
This article first appeared in the Wisconsin Health News daily email newsletter. Sign up for your free trial here.





