
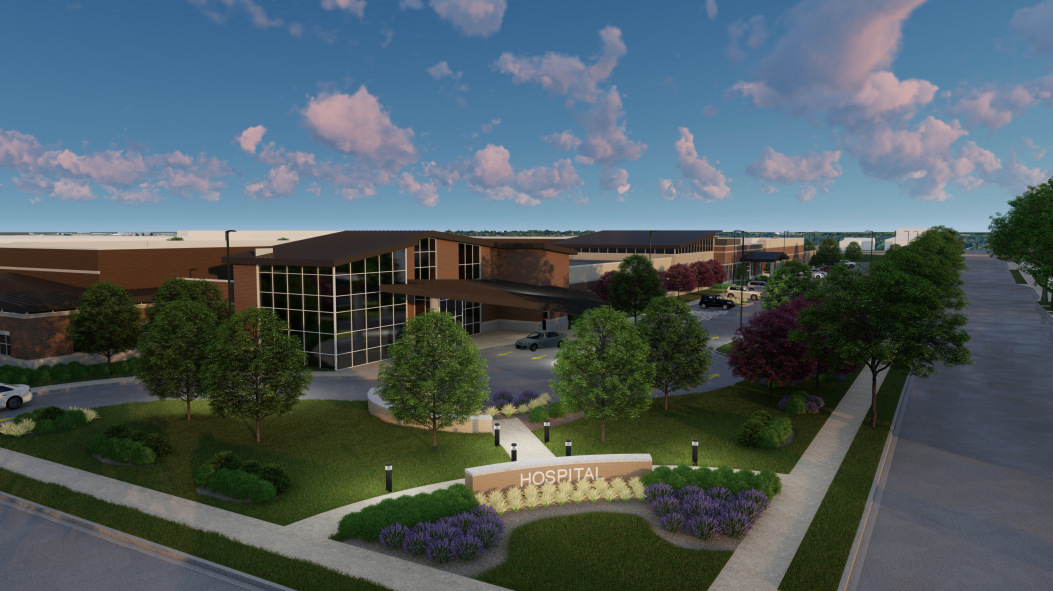
Universal Health Services plans first Wisconsin hospital
Pennsylvania-based Universal Health Services is planning its first behavioral health hospital in Wisconsin.
The proposed West Allis facility will serve residents in southeast Wisconsin and those referred from Milwaukee County’s Behavioral Health Division.
“It’s really important to us to be a strong contributor in whatever communities we’re in and to have a strong local presence,” said Diane Henneman, UHS divisional vice president. That includes hiring a CEO for the hospital who’s hopefully from the community, she said.
The new facility will include an indoor gymnasium and enclosed courtyards. UHS will provide care across multiple disciplines, Henneman said.
Henneman recently spoke to Wisconsin Health News. Edited excerpts are below.
WHN: UHS did a study to determine need in the area. What did the study find in terms of need?
DH: We did a bed need analysis, which is what we typically do whenever we go into a new market or even in some of our existing markets where it seems like demand is outpacing need. We like to do it at a 40-mile radius and a 60-mile radius of the location. At both, it really showed a significant need for adult and older adult services at the inpatient level of care and then also child and adolescent services. That’s our plan for the new facility – to provide inpatient treatment for all three of those populations in separate units and separate programming.
WHN: What services will the facility be providing?
DH: We will serve really all ages of people who need an inpatient level of care…really we will end up treating the full range of individuals who are in a mental health crisis. Our older adult unit will be specialized. Our child and adolescent unit will be specialized. And then because we will have three general adult psychiatric units, we will be able to differentiate maybe by gender or by type of illness that you’re dealing with. And then we’ll also offer partial hospitalization and intensive outpatient services at the hospital. So if someone’s done with their inpatient treatment and they want to step down to kind of an intermediate step between being hospitalized and going to back to your outpatient provider, they would have that ability too.
WHN: How does the need for behavioral health treatment for older adults compare to other types of behavioral health needs?
DH: I think it depends by the community you’re in. I think as the general population gets older, more specialized services for older adults are needed and not everyone is comfortable working with that population or has that area of expertise. But it kind of varies market to market. What we see in most of the communities that we are in is just a significant shortage of inpatient beds and a lot of people languishing in ERs or in other settings unable to really access services quickly, in an efficient manner, close to home. We sometimes have people coming four or five hours for a hospital because it’s the closest service available to them and that’s really difficult for families to participate in treatment.
WHN: A number of providers considered taking on the inpatient services provided by the Behavioral Health Division in recent years but decided against submitting a proposal. Why did you decide to take on these services?
DH: For us, it’s our core business – it’s our area of expertise. UHS has over 250 behavioral health facilities throughout the United States. We have about 1,800 beds in the United Kingdom. And we’re a company that’s been in the behavioral health business for 40 years. So we’re very comfortable treating those populations and treating the needs of the local communities. For us, it seemed like a good fit with what we feel our primary skill set is and what we have to offer. The county seemed receptive and the community seems receptive to working with us as a provider. It looked like a good opportunity.
WHN: The facility won’t have a psychiatric emergency room. Is UHS planning to work with the county and local providers on their efforts to reform crisis care in the county?
DH: We’ve been involved a little bit and we’ll continue to be involved as much as we can in helping with that. But building a new hospital is a fairly significant endeavor. That is our primary, our core business, our core competencies. That’s really what we felt like we could contribute to the community at the time and trying to do both of those things seemed like it would be a lot. It didn’t seem like you could do both of these things at the same time, especially being a new provider in the community. But I anticipate working with (Behavioral Health Division Administrator) Mike Lappen and BHD and the Milwaukee Health Care Partnership on what other ideas we have, strategies we can help contribute to in terms of how that ends up being redesigned.
WHN: There’s a shortage of mental healthcare providers in the state. How do you plan to address that when hiring?
DH: We’ve had to deal with that in a lot of states, in a lot of different markets. I think that’s one of the advantages of being a national company with such a broad reach. We will do local recruiting and national recruiting. We have a lot of resources that we’ll bring to the table to source candidates at all levels. We’ll work with the county in terms of their employees who might be interested in working for us once the new hospital is open. We’ll look at all the types of residency programs and internships that you see. We have all those at our hospitals. That’s often a good feeder for us in terms of employees. But we have been pretty successful in our recruitment and retention efforts across our company. We’ll bring those same strategies here to work with all the local talent here and hire the best people for the hospital.
WHN: Are you planning to give preference to hiring from the county’s current inpatient hospital?
DH: We’re planning a preferential interviewing process, kind of streamlined access to our HR team and our recruiters if people are interested in coming over, and some sessions before the hospital is open around information gathering and getting to know UHS as an employer. We have a number of those things. It’s a little early now obviously, because we haven’t broken ground. That’s definitely on the horizon for us when working with BHD.
WHN: What are the next steps going forward?
DH: We just submitted the request to purchase the land and the plan design approval with the City of West Allis. So we’ll go through that approval process, which can take a couple of months it looks like. And hopefully, that will go favorably, and then we’ll finish the really detailed design of the hospital. We have a best practice prototype we follow in designing our hospitals, but it also has to fit the land that you’re building on. The best case scenario, we’ll be starting construction at the end of the year potentially and opening in 2021.
This article first appeared in the Wisconsin Health News daily email newsletter. Sign up for your free trial here.





